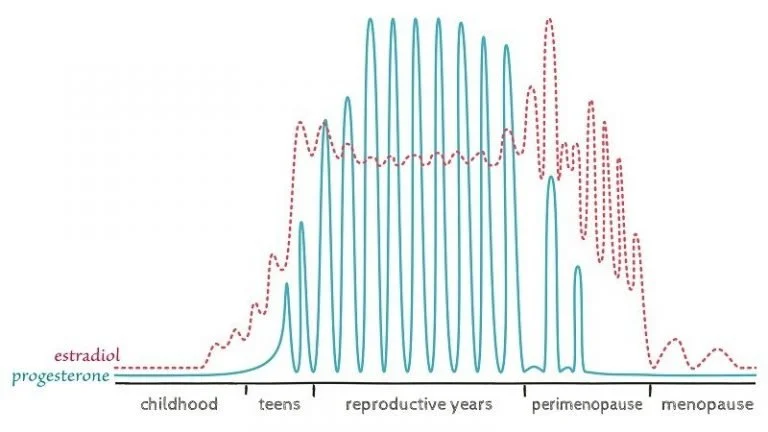
Diagram from Lara Briden’s Hormone Repair Manual
Perimenopause is a gradual transition that typically begins in a woman's 40s, marking the lead-up to menopause. It's important to note that for women over 45, perimenopause is typically a clinical diagnosis and does not require lab assessment for confirmation. To help you recognize if you're entering this phase, here are some key signs to look out for:
Changes in menstrual patterns: Your periods may become irregular, with cycles becoming longer or shorter. You might still have periods, but the consistency and frequency may vary. Often your period becomes shorter before it gets less frequent.
New physical symptoms: You may experience hot flashes, night sweats, or changes in your skin and hair. Vulvar and vaginal symptoms can also occur while you're still menstruating. You may also have an exacerbation of pre-existing symptoms such as breast tenderness.
Insomnia and sleep changes: As your hormones fluctuate your sensitivity to that could cause worsening of sleep, either a few days before your period or throughout the cycle.
Mood changes: Some women notice shifts in their emotional state, including increased irritability or mood swings. It's important to note that while mood changes are common, severe depression should be addressed with a healthcare provider.
To better understand and manage your perimenopause journey:
Track your symptoms: Keep a record of your menstrual cycles and any new symptoms you experience. This can help you identify patterns and provide valuable information to your healthcare provider.
Get appropriate testing: Again hormone testing does not diagnose perimenopause however getting baselines of B12, ferritin, liver enzymes, lipid panels can be helpful to assess your overall health and cardiovascular risk (one thing we care about the most!)
Consider your family history: Ask your mother about her menopause experience, as there can be genetic similarities. Ask about family history of osteoporosis and cardiovascular disease. These areas of health are important to monitor in women’s health.
Seek expert help: Consider seeing a menopause practitioner who specializes in this life stage to get targeted support and avoid misdiagnosis.
Remember, every woman's experience with perimenopause is unique. By staying informed and proactive about your health, you can navigate this transition more smoothly and ensure you receive appropriate care and support.